Abstract
Background
The immune system has been shown to be important in the pathophysiology of MDS. Adaptive immunity relies on T cells ability to discriminate between self and non-self antigens in the context of a surface bound MHC protein structure. Genomic changes occurring in acquired somatic mutations can encode novel amino acid sequences, which if translated and presented by the MHC are termed a neoantigen.
To establish the impact of neoantigens in MDS we have combined a predictive algorithm to screen cases for the presence of neoantigens together with mass cytometry by time of flight (CyTOF) to identify neoantigen-related immune signatures.
Results
Mutation screening was performed on 204 MDS patients using our established gene panel targeting mutations commonly occurring in MDS (Mohemdali, Leukaemia 2015). Neoantigen-MHC affinity was predicted using NetMHCpan3.0 with neoantigen affinities ranked against 400,000 naturally occurring peptides. Those in the top 2% of peptides were classed as predicted neoantigens.
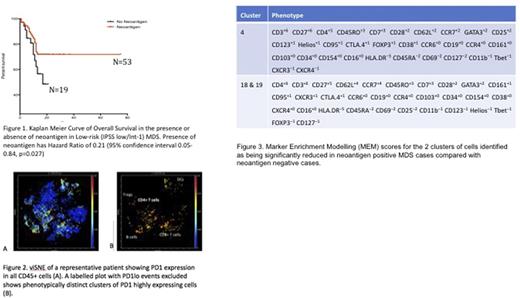
In a multi-variate analysis of overall survival, higher numbers of mutations were associated with a poorer outcome (HR 2.71 95%CI 1.28-5.73, p <0.01). In a subset of 72 low risk MDS cases (by IPSS) the presence of neoantigen was protective (HR 0.21 95% CI 0.05-0.84, p <0.05) (fig 1). There was no survival benefit in the presence of neoantigens in high risk MDS.
To look for an immune signature in MDS, we performed deep immunophenotyping on 44 MDS cases and 8 age-matched healthy donors (HDs). Peripheral blood mononuclear cells (PBMCs) were stained with 35 metal-tagged antibodies and analysed using CyTOF. Automated clustering methods (t-distributed stochastic neighbour embedding (t-SNE), spanning-tree progression analysis of density-normalized events (SPADE) and in-house clustering) were used to identify T cell subsets. As expected, T regulatory cells were increased in MDS cases when compared to HDs (7.2% vs 4.9% p <0.00001). However, within MDS there was an increase in the recently described Treg B (Kordasti, Blood 2016) in RAEB (4.9% vs 3.6%, p <0.05). These Tregs have been shown to be activated, more suppressive, quicker in responding to IL-2 by phosphorylating STAT5 and Treg specific demethylated region (TSDR) is unmethylated. Of note, there was no difference in abundance of Tregs or other T cell subsets based on presence or absence of mutation or neoantigen.
To assess other features of immune suppression we analysed expression of immune checkpoints. While there was no difference in percentage of PD1 positive cells as a proportion of T cells between MDS and HD, neoantigen positive patients had higher PD1+ T cells compared to negative cases (0.77 vs 1.69% p <0.005). To explore the phenotype of PD1 positive PBMCs further we used unsupervised clustering and identified 23 phenotypically distinct clusters of PD1 high cells (fig 2). Neoantigen positive cases had significantly lower numbers of two distinct PD1hi CD4+ T cell subsets (p<0.05). Using Marker Enrichment Modelling (MEM) to better characterise these clusters, we have shown one cluster to be part of the Treg B subpopulation and the other within T effectors (fig 3) (Diggins, Nature Methods 2017). No significant differences in numbers of these cells was seen between other subtypes of MDS, including presence or absence of mutations, or between MDS and HD.
Discussion
Using multi-dimensional analysis we have shown that increased blast counts are associated with an increase in more suppressive and proliferating Tregs (Treg B). The findings of increased numbers of PD1hi T-cells and also two specific CD4+ subsets implies a more immunosenescent phenotype in neoantigen negative MDS. The lack of this association when comparing mutation positive and negative cases suggests that this immune signature is dependent on the patient-specific interaction of the mutation with HLA type rather than driven by the presence of a mutation per se.
This work demonstrates clearly for the first time the protective role of neoantigens in low risk MDS. By combining knowledge of host immune factors and tumour characteristics we have identified two novel subsets of PD1 upregulated CD4+ T cells that may play an important role in tumour surveillance and identifies cells likely to be susceptible to PD1 blockade. Further work to understand the mechanistic effects of PD1 blockade on these subsets will be crucial to identifying patients most likely to respond to checkpoint inhibition.
Kulasekararaj: Akari Therapeutics Plc: Consultancy, Honoraria; Alexion Pharmaceuticals: Consultancy, Honoraria; Ra Pharmaceuticals: Consultancy, Honoraria; Achillion pharmaceuticals: Consultancy, Honoraria. Irish: Cytobank Inc: Equity Ownership, Membership on an entity's Board of Directors or advisory committees; Janssen: Research Funding; Incyte: Research Funding. Kordasti: Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal